By Ilyana Rosenberg
August 2, 2020
The Coronavirus forced organizations around the globe to suddenly suspend elective testing and procedures during its rapid, highly transmissible outbreak. A study conducted by Strata Decision Technology (Strata) reveals a decrease of 54.5% in the number of patients who sought care in a hospital setting when comparing a two-week period between March and April 2019 versus March and April 2020. The analysis included 228 hospitals, encompassing 51 health care delivery systems that span 40 states.
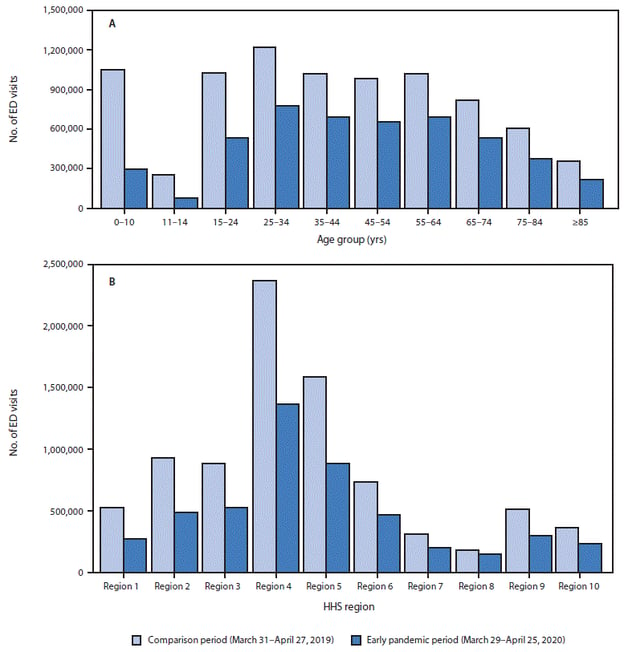
FAIR Health reports that hospitals in the Northeast realized a 26% decline in average per-facility revenues when compared to the same reporting period in 2019. FAIR Health’s second survey: Illuminating the Impact of Covid-19 on Hospitals and Health Systems: A Comparative Study of Revenue and Utilization uncovers that the third week of March witnessed thousands of new Covid-19 cases in certain parts of the United States, most commonly in the Northeast. This surge in positive Coronavirus cases directly impacted the number of emergency department encounters per day. According to the June 12, 2020, weekly report from the Centers for Disease Control and Prevention (CDC), the number of ED visits decreased 42% per week during the early pandemic period of March 29-April 25, 2020.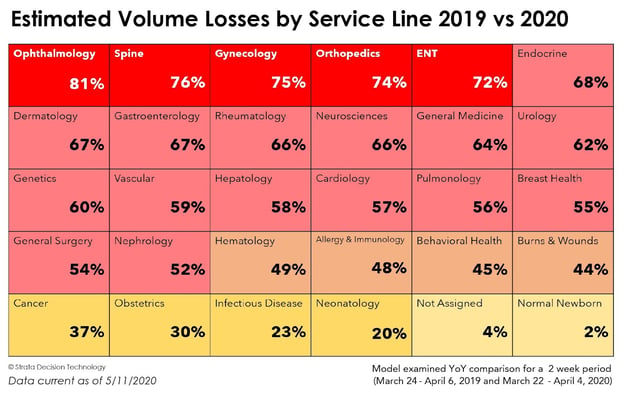
The CDC further defines the decrease in emergency department visits by age group and region:
Restrictions are gradually being lifted on elective testing and procedures. Hospitals are permitted to diagnose and treat non-emergent conditions, provided they have sufficient personal protective equipment (PPE) for front-line medical workers who could be exposed to COVID-19.
Most states have implemented a phased approach to opening elective procedures in an attempt to eliminate the risk of exposure. Other common state-to-state requirements include:It is anticipated that the reinstatement of elective procedures will produce a mass increase in patient volumes. Millions of patients are awaiting care or the rescheduling of non-emergent procedures that were previously delayed in order to comply with state-specific COVID-19 restrictions. As states re-open elective procedures, facilities will likely be challenged by the surge in patient volumes while also maintaining capacity and social distancing requirements for COVID-19 patients.
Although no comprehensive survey data is available, it is likely that backlog and COVID specific coding challenges are arising as a result of the spike and fluctuation. While there is no solution in sight yet for pandemic induced spikes and their effect on the front line, we know that we can rely on the scale-flexibility and consistency of new automated coding technology to help with the back-office consequences.
Autonomous coding is a fully automatic artificial intelligence solution that requires no human intervention. It understands unstructured physician language and can explain the rationale behind each code assigned. Autonomous coding solutions provide significant value to healthcare and revenue cycle management organizations. A fully automated coding solution offers:
The COVID pandemic has created significant challenges for health care organizations around the world. The fluctuation in volumes and subsequent furloughs, terminations, and layoffs have made it difficult for revenue cycle leaders to meet key performance indicators such as productivity, quality, and expected turnaround times. Autonomous coding offers a seamless, cost-effective solution for reducing backlog, improving quality scores, and increasing speed to revenue.
For inquiries about partnering with Nym please contact us.

Product Management